So, You’ve been diagnosed with Hashimoto’s, what now?
Many Hashimoto’s diagnoses sound something like this “We received the results of your blood tests. You’ve been diagnosed with Hashimoto’s thyroiditis. Eventually, your thyroid function will decline, and you will be on thyroxine for the rest of your life. There is nothing you can do. Simply take medication.” This was my diagnosis, and my doc delivered the news just like that.
We are fortunate to have access to both conventional medicine and functional nutrition, both of which may assist you in managing your illness. Speaking from personal experience, a diagnosis of Hashimoto’s disease may seem like the end of the world, but believe me when I say it is not a life sentence of weight gain, tiredness, dry skin, hair loss, and constipation. Instead, we can manage this condition with diet and exercise. Using both conventional and naturopathic techniques, we have a vast array of tools at our disposal to support your thyroid function, lower antibody titers, relieve your symptoms, and guarantee that you continue to feel energetic and vital in the long run.
So let, dive into the world of living with Hashimotoʼs.
According to the World Health Organization, thyroid diseases are more common than you may think, affecting millions of individuals worldwide every year. I know many people can relate to this because, according to the American Association of Clinical Endocrinologists, more than 30 million Americans suffer from thyroid dysfunction, half of whom go undiagnosed by conventional medicine (1) Of the detected cases of hypothyroidism, 90 percent are due to Hashimoto’s disease.
Although many people have an official diagnosis, many are unaware of what it truly entails. And yet, specialists may tell you your thyroid function will gradually degrade, but it would require a lifetime routine of medications. Fortunately, there are things you can do to prevent flare-ups of the disease. Natural medicine provides an abundance of methods you can incorporate into daily habits to maintain thyroid function. These techniques can lower autoimmune antibody titers, reduce symptoms, and ensure that you stay in control of your health and your life. It all boils down to properly educating yourself and taking responsibility for your health.
What is Hashimoto’s?
Hashimoto’s disease is an autoimmune disorder where the body produces a specialized white blood cell (lymphocyte) that attacks the thyroid gland. Your thyroid, therefore, produces less thyroid hormone, generally to the point where you need to take a synthetic hormone replacement, such as thyroxine. It is among the most common causes of underactive thyroid in third-world countries, also known as hypothyroidism. 1 Because thyroid hormones govern metabolism, many of the body’s functions become sluggish when the thyroid hormone levels are low.
Hashimoto’s disease affects more women than men, with a male-to-female ratio of at least 10:1. Most thyroid illness diagnoses occur between 30 and 50 years of age; however, the likelihood and prevalence of thyroid disease increase with age in general. Pregnancy is another significant risk factor due to the mother and fetus’s high iodine requirements. The changes in reproductive hormones produce variations in thyroid hormone levels throughout pregnancy. Some women produce antibodies to their thyroid, resulting in a disorder known as postpartum autoimmune or subacute thyroiditis. Hashimoto’s disease is related to various other autoimmune conditions, including pernicious anemia, vitiligo, diabetes mellitus, Addison’s disease, rheumatoid arthritis, and celiac disease (2).
Symptoms of Hashimoto’s
During the initial stages, patients may experience the symptoms of excess thyroid hormone known as Hyperthyroidism. Symptoms may include racing heartbeats, anxiety and hyperactivity, heat sensitivity, sweating, and weight loss, among several other indicators. When the thyroid gland becomes inflamed, this induces the gland to release a large amount of previously-stored thyroid hormone, causing Hyperthyroidism. Over time, the thyroid gland will essentially exhaust itself out, and the hyperthyroid symptoms will give way to hypothyroid symptoms such as:
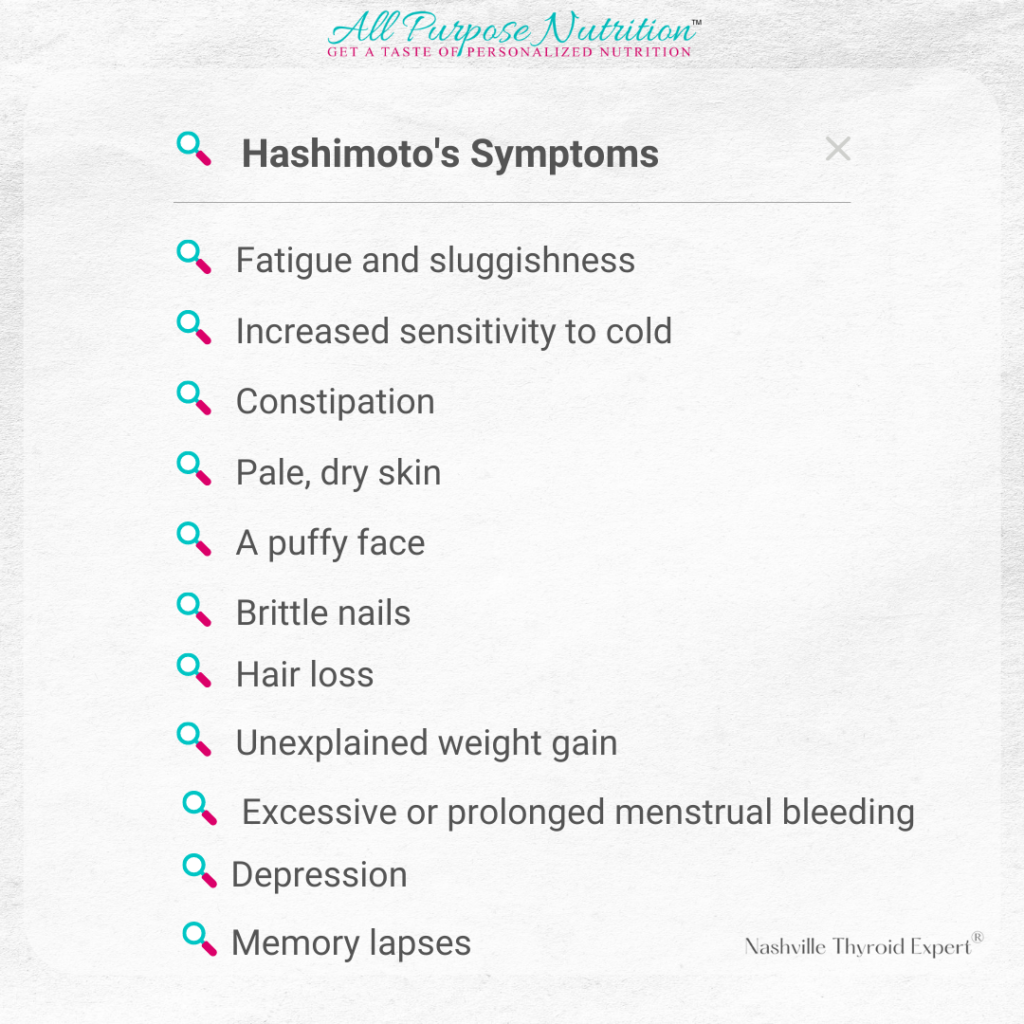
An enlarged thyroid gland, typically referred to as a goiter, is a common complication of Hashimoto’s thyroiditis. As the disease impairs the thyroid’s ability to operate, the thyroid will continue to grow.
Diagnosis
Many doctors will merely order a TSH (thyroid-stimulating hormone) test then call it a day with no further action. Doing so may exclude essential information and leave you with a slew of questions. It is critical to do extensive thyroid blood tests to assess your overall thyroid function. Such examinations may include; T4, free T4 (the inactive form of thyroid hormone), T3 (the active form of thyroid hormone), reverse T3, TSH, and thyroid autoantibodies. These tests reveal which hormones your thyroid produces, in what amounts, and whether the hormones are converting effectively.
Your physician may not establish a diagnosis until well into the illness due to the continuous complexity of Hashimoto. According to one study, autoantibodies in autoimmune diseases are often present for several years before a diagnosis can be determined. (3) Testing may be necessary for those with several risk factors for Hashimoto’s disease to avoid the thyroid gland from being destroyed. The most typical test results show an elevated TSH, low concentrations of free T4, and an increase in thyroid peroxidase antibodies.
Causes of Hashimoto’s
The causes of Hashimoto’s disease are still not well understood. Research reveals several likely environmental and nutritional reasons, potentially triggering the onset and progression of the disease. These include:
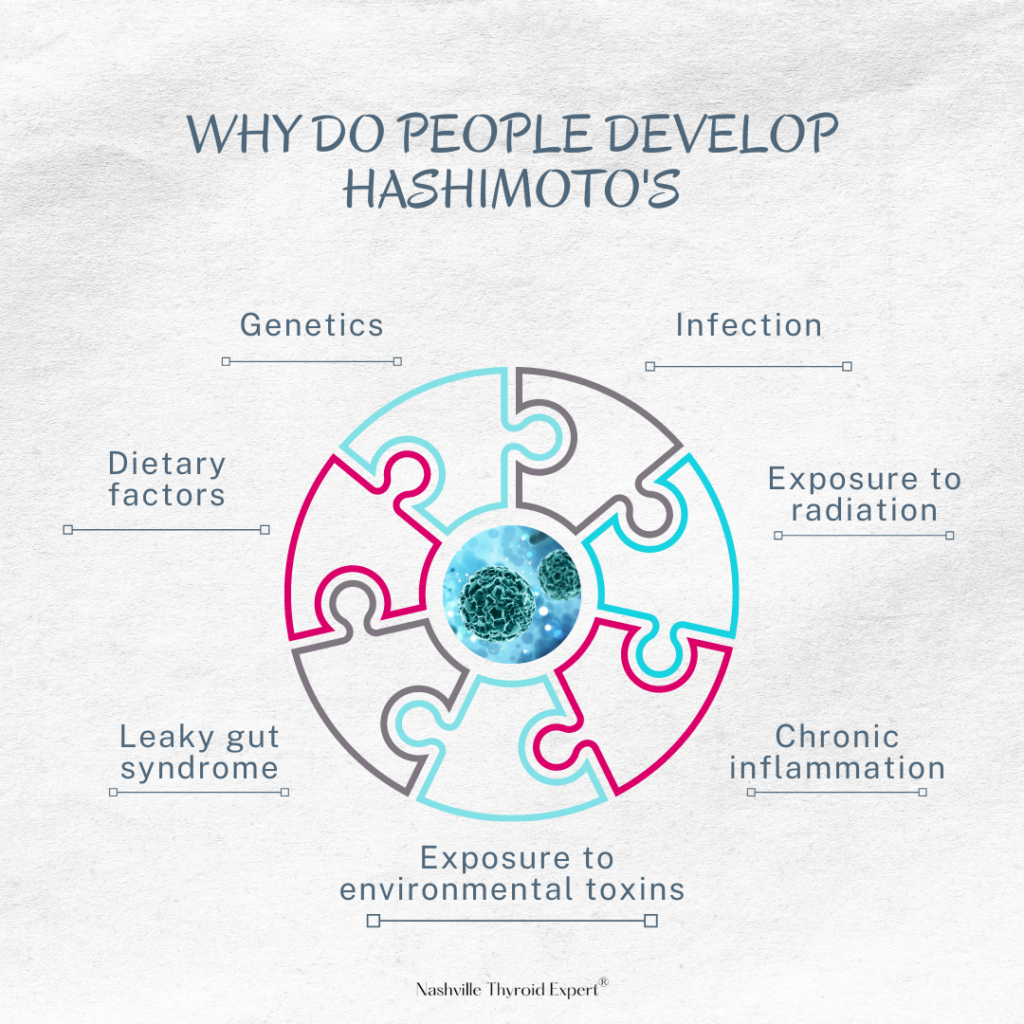
Genetics
Cases reveal genetics being a significant factor in Hashimoto’s illness. Twin studies indicate that between 70% and 80% of vulnerability to autoimmune thyroid disease is genetic. (4) There is almost always an underlying biological component and a trigger that sparks off a chain of events resulting in Hashimoto’s disease. Susceptibility to Grave’s disease, another autoimmune thyroid illness, is equally conferred by the underlying genetic predisposition.
Infections
Infections from parasites, viruses, and bacteria have all exposed links to the development of Hashimoto’s illness. Hepatitis C, for example, is directly related to thyroid autoimmunity and hypothyroidism across several studies. (5) Inflammation generated by a viral infection may result in the activation of T cells, which then contribute to the development of autoimmunity. Molecular mimicry, which defines a compositional resemblance between viral and self-antigens, may also be a causative mechanism. This process leads to the body attacking its tissues.
Multiple outside viruses may contribute to the onset of Hashimoto. Including parvovirus rubella, herpes simplex virus, Epstein Barr virus, and human T lymphotropic virus type 1. (6). Numerous studies also indicate a link between Toxoplasma gondii infection and a rise in thyroid autoantibodies. Further analysis will be required before officials can take any action to confirm the findings.
Environmental toxins and chemicals
Environmental pollutants and chemicals are studied and found to enhance the probability of developing autoimmune thyroid disease. Natural toxins are organics made from coal and in the air and water, including polyhalogenated biphenyls (PBB) and polyaromatic hydrocarbons (PAHs). These toxins demonstrate promoting thyroid autoimmunity in genetically predisposed people. (8) PBB compounds are utilized in various industrial applications, including flame retardants, lubricants, adhesives, and plasticizers. Other chemicals with high oestrogenic characteristics, such as Bisphenol A, have been linked to disruptions with thyroid hormone production and conversion. (9)
Heavy metals, particularly aluminum, lead, cadmium, and mercury, can cause significant thyroid damage. Deodorant, over-the-counter drugs like antacids, food additives, cookware, and vaccines all contain aluminum. Aluminum oxidizes the thyroid, inhibits iodide consumption and thyroid hormone production, and triggers an autoimmune reaction. Researchers discovered cadmium’s presence in thyroid hypertrophy and nodules. Cadmium is found in batteries, plastics, sewage, and phosphate-based fertilizers due to mining and smelting activities. Lead poisoning has long been considered harmful, and it has been related to decreased thyroid function and increased thyroid-stimulating hormone levels. Paint, ceramics, newspaper, solder, dolomite, and pewterware are just some environmental lead sources. Mercury can limit iodine intake and lower TSH production. Seafood, dental amalgams, fungicides, mining, paints, explosives, batteries, fluorescent lamps, cosmetics, hair colors, and petroleum products have traces of mercury. These metals all assist with the development of Hashimoto and other autoimmune diseases.
Drugs
Certain pharmaceuticals may cause exacerbation of Hashimoto’s disease in some people. For instance, interferon (IFN-) is a drug used to treat chronic hepatitis but was observed in various thyroid autoimmunity diseases. (11) Similarly, IL-2 is used to treat melanoma and kidney cancer but can potentially cause hypothyroidism and thyroid autoantibodies. (12) Lithium may raise the likelihood of hypothyroidism in patients with autoimmune thyroid disease. Exposure to Lithium is likely to increase thyroid antibody titers and the incidence of thyroid autoimmunity. (13) The effects of Amiodarone, used to treat cardiac arrhythmias on the thyroid, have long been recognized in medical studies. Amiodarone’s structural resemblance to thyroid hormones and its high concentration of Iodine may contribute to thyroid dysfunction. (14)
Poor Gut Health- Intestinal Permeability and Food Sensitivities
Many people are unaware that there is a strong link between gut health and thyroid function. Research has revealed that a chronic persistent microbiota imbalance and inflammation in the gut are key contributing factors to general autoimmune diseases, like Hashimoto. Immune cells reside in the gut to the extent of 70-80%, and intestinal bacteria play a vital part in converting T4 to T3 in the body. In addition, intestinal permeability, often known as leaky gut, has been associated with Hashimoto’s thyroiditis. In cases where the gut wall is porous or leaky, the bloodstream becomes exposed to potentially hazardous foreign chemicals and food proteins to which you may be allergic. The immune system then responds with an inflammatory response, responding with a possible incorrect immunological attack on the body’s tissues. A thyroid gland is a clear outcome of this disruption. It is possible that inflammation in the gut can raise cortisol levels and that elevated cortisol will degrade T4 to T3.
Vitamin D deficiency
Vitamin D is not only essential for assisting your body in the absorption of calcium and the strengthening of your bones, but it’s crucial in maintaining the delicate equilibrium of your immune system. According to studies, autoimmune disorders are more common in regions further away from the equator. One of the possible causes for this could be related to insufficient vitamin D levels. In various autoimmune disorders, including Hashimoto’s thyroiditis, low vitamin D levels are frequent findings. (15) Patients with autoimmune thyroid diseases, those related to anti-thyroid antibodies and impaired thyroid function, were documented to have significantly low vitamin D levels. Studies including vitamin D supplementation observed a decrease in thyroid antibodies. This recognition proves that vitamin D is highly beneficial in slowing down and avoiding the progression of Hashimoto’s disease.
Iodine Intake
Increased iodine consumption (in some cases, iodine insufficiency) is another factor connecting the development of Hashimoto’s thyroiditis. A building block for thyroid hormones is Iodine, and due to the particular way iodine processes in the body, it becomes a problem for some. When Iodine is consumed or taken in supplement form, it goes through phases involving the hypothalamus, pituitary, and thyroid gland. (16) Throughout this reaction, hydrogen peroxide, a free radical, is released into the environment. The body requires an adequate amount of selenium (17) to neutralize hydrogen peroxide in the bloodstream. Consequently, if one does not have appropriate selenium levels or excessive amounts of Iodine, the hydrogen peroxide can trigger early damage and programmed cell death in thyroid tissues. (18) These iodine-overloaded cells are therefore capable of activating the autoimmune process in those genetically prone to it.
Stress
Stress is one of the most underestimated triggers, particularly for thyroid autoimmunity, because Hashimoto’s disease is gradual. Numerous studies have revealed that psychological and physiological stressors induce various changes in the immune system, either indirectly or directly, through the neurological (nervous) and endocrine systems. (19) When you are under stress, your hypothalamus sends a signal to your pituitary gland, which sends an alert to your adrenal glands, causing them to generate and release stress hormones, including cortisol. Your body enters a state of “fight or flight,” and your stress hormones cause your body’s routine functions to reprioritize to deal with the stressor in front of you. Among them are digestion, immunological response, thyroid hormone production, and the conversion of thyroid hormone from type 4 to type 3.
These immune modulations and the effect on the thyroid may contribute to the development of autoimmunity in genetically predisposed individuals.
Treating Hashimoto’s Naturally
Diet
- Avoid gluten- studies have shown an association between sensitivity to gluten-containing products and autoimmune thyroid problems, including Hashimoto’s. Research has also found that a significant number of patients with Hashimoto’s also have coeliac disease. (20)
- It’s also good to consider undergoing a more comprehensive elimination diet of the major allergens and sensitivities, including dairy, eggs, nightshade vegetables such as eggplants and tomatoes, soy, and sugar, as well as avoiding caffeine and alcohol. These products are known to disturb thyroid hormone production as it suppresses the body’s ability to use thyroid hormone. (21)
- Avoid food additives and chemicals and all refined foods, mainly processed grains and sugars, as well as all products containing aspartame. In the body, aspartame metabolizes into the toxic substance formaldehyde, which the liver cannot clear. Thus, it remains lodged, causing inflammation and becoming a potential for autoimmune issues such as Hashimoto’s thyroiditis. (22)
- Incorporating selenium-rich foods such as Brazil nuts is beneficial as it is essential for thyroid function.
- Iodine- before increasing iodine-rich food such as seaweed and iodized salt, it is crucial to check your levels as excess iodine consumption can trigger or exacerbate Hashimoto’s.
- Antioxidant-rich foods- are necessary to fight the free radical damage caused by inflammation. Emphasis on vitamin A containing foods, it’s imperative, as vitamin A is often deficient in people with any autoimmune condition. Antioxidant-rich foods include berries, apples, nuts such as pecans, beams, red cabbage, beetroot, and dark leafy greens.
- Healthy fats- are vital to helping decrease inflammation actively, and they will also provide another energy source for the body. They can be found in avocados, olive oil, nuts, and seeds, especially walnuts and chia seeds.
- Probiotic foods- increase probiotic-rich foods such as kombucha, sauerkraut, non-dairy kefir and yogurt, and kimchi to provide beneficial bacteria in your gut which is essential for modulating your immune response.
- In cases of iodine deficiency, you should avoid raw vegetables from the brassica family. They release goitrogenic chemicals, which can compete with iodine uptake in the thyroid and interfere with thyroid hormone synthesis. Including vegetables such as broccoli, cauliflower, brussels sprouts, kale, cabbage, and more. However, if iodine intake is sufficient, strict avoidance is not recommended as many of these foods have beneficial properties. Steaming or boiling them reduces their goitrogenic effect.
Lifestyle
Given the vast amount of toxins in the environment, which can interfere with thyroid function, it is important to reduce your exposure to environmental toxins as much as possible. Here are some tips to get you started as well as some other essential lifestyle tips:
- Buy organic food as much as possible to avoid toxic agricultural agents and peel non-organic fruits and vegetables
- Stop using pesticides, herbicides, and fungicides (or fertilizers that contain them) in the yard and garden
- Convert to all-natural personal hygiene products and cosmetics that are free of heavy metals and other toxic compounds
- Use chemical-free, biodegradable laundry, and household cleaning products and choose chlorine-free products and unbleached paper products (i.e., tampons, menstrual pads, toilet paper, paper towel, coffee filters).
- Limit the use of plastic containers for drinking and food storage or at least opt for BPA-free varieties
- Invest in a quality water filter
- Replace non-stick cookware items with stainless steel or cast-iron options
- Reduce stress: As previously stated, stress can interfere with the body’s ability to heal itself and exacerbate an autoimmune inflammation response. You may be able to alleviate the symptoms of Hashimoto’s and lessen the severity by implementing stress management practices such as a regular sleep schedule, massage, meditation, and yoga and managing stress with herbal and nutritional supplements, as described above.
- Participate in frequent physical activity since it not only prevents areas in weight gain, sleep disturbances, and anxiety, it also reduces inflammation and improves symptoms of Hashimoto’s.
Supplements
Lab tests should be performed every 3-6 months in order to monitor thyroid hormone levels. Medication or supplemental adjustments should be made accordingly. It is highly prescribed to consult a health practitioner to know exactly what to supplement and how much but common prescriptions include:
- Vitamin D for immune regulation
Trace minerals such as selenium, zinc, iodine, chromium, and manganese for peripheral thyroid hormone conversion. Be cautious supplementing iodine and selenium, though. - Omega 3 fatty acids to reduce inflammation
- Digestive enzymes to aid with absorption
- B vitamins to help support energy production which is often depleted in Hashimoto’s.
- L-glutamine for intestinal permeability and to aid cellular repair
- Probiotics, best to get a broad spectrum or rotate for different strain coverage
- Adaptogenic herbs such as Withania, Rhodiola, and Licorice to balance adrenal function and aid with the peripheral conversion of T4 to T3
- Anti-inflammatory herbs such as turmeric help reduce inflammation as well as support the liver
- Glutathione– for its potent antioxidant activity
Ready to Get Rid of Your Hypothyroid Symptoms?
Check out these resources that can help you.
References
- Mincer, D.L & Jialal, I. (2020). Hashimoto Thyroiditis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459262/
- Mincer, D.L & Jialal, I. (2020). Hashimoto Thyroiditis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459262/
- Arbuckle, M. R., McClain, M. T., Rubertone, M. V., Scofield, R. H., Dennis, G. J., James, J. A., & Harley, J. B. (2003). Development of autoantibodies before the clinical onset of systemic lupus erythematosus. The New England journal of medicine, 349(16), 1526–1533. https://doi.org/10.1056/NEJMoa021933
- Hansen, P. S., Brix, T. H., Iachine, I., Kyvik, K. O., & Hegedüs, L. (2006). The relative importance of genetic and environmental effects for the early stages of thyroid autoimmunity: a study of healthy Danish twins. European journal of endocrinology, 154(1), 29–38. https://doi.org/10.1530/eje.1.02060
- Zaletel, K., & Gaberšček, S. (2011). Hashimoto’s Thyroiditis: From Genes to the Disease. Current genomics, 12(8), 576–588. https://doi.org/10.2174/138920211798120763
- Desailloud, R., & Hober, D. (2009). Viruses and thyroiditis: an update. Virology journal, 6, 5. https://doi.org/10.1186/1743-422X-6-5
- Kaňková, Š., Procházková, L., Flegr, J., Calda, P., Springer, D., & Potluková, E. (2014). Effects of latent toxoplasmosis on autoimmune thyroid diseases in pregnancy. PloS one, 9(10), e110878. https://doi.org/10.1371/journal.pone.0110878
- Lindsay, R. H., Hill, J. B., Gaitan, E., Cooksey, R. C., & Jolley, R. L. (1992). Antithyroid effects of coal-derived pollutants. Journal of toxicology and environmental health, 37(4), 467–481. https://doi.org/10.1080/15287399209531686
- Moriyama, K., Tagami, T., Akamizu, T., Usui, T., Saijo, M., Kanamoto, N., Hataya, Y., Shimatsu, A., Kuzuya, H. & Nakao, K. (2002). Thyroid Hormone Action Is Disrupted by Bisphenol A as an Antagonist, The Journal of Clinical Endocrinology & Metabolism, 87(11): 5185–5190, https://doi.org/10.1210/jc.2002-020209
- Chen, A., Kim, S. S., Chung, E., & Dietrich, K. N. (2013). Thyroid hormones in relation to lead, mercury, and cadmium exposure in the National Health and Nutrition Examination Survey, 2007-2008. Environmental health perspectives, 121(2), 181–186. https://doi.org/10.1289/ehp.1205239
- Tomer Y. (2010). Hepatitis C and interferon induced thyroiditis. Journal of autoimmunity, 34(3), J322–J326. https://doi.org/10.1016/j.jaut.2009.11.008
- Barbesino G. (2010). Drugs affecting thyroid function. Thyroid : official journal of the American Thyroid Association, 20(7), 763–770. https://doi.org/10.1089/thy.2010.1635
- Baethge, C., Blumentritt, H., Berghöfer, A., Bschor, T., Glenn, T., Adli, M., Schlattmann, P., Bauer, M., & Finke, R. (2005). Long-term lithium treatment and thyroid antibodies: a controlled study. Journal of psychiatry & neuroscience : JPN, 30(6), 423–427.
- Danzi, S., & Klein, I. (2015). Amiodarone-induced thyroid dysfunction. Journal of intensive care medicine, 30(4), 179–185. https://doi.org/10.1177/0885066613503278
- Kivity, S., Agmon-Levin, N., Zisappl, M., Shapira, Y., Nagy, E. V., Dankó, K., Szekanecz, Z., Langevitz, P., & Shoenfeld, Y. (2011). Vitamin D and autoimmune thyroid diseases. Cellular & molecular immunology, 8(3), 243–247. https://doi.org/10.1038/cmi.2010.73
- Ahad, F., & Ganie, S. A. (2010). Iodine, Iodine metabolism and Iodine deficiency disorders revisited. Indian journal of endocrinology and metabolism, 14(1), 13–17.
- Contempre, B., Dumont, J. E., Ngo, B., Thilly, C. H., Diplock, A. T., & Vanderpas, J. (1991). Effect of selenium supplementation in hypothyroid subjects of an iodine and selenium deficient area: the possible danger of indiscriminate supplementation of iodine-deficient subjects with selenium. The Journal of clinical endocrinology and metabolism, 73(1), 213–215. https://doi.org/10.1210/jcem-73-1-213
- Xu, J., Liu, X. L., Yang, X. F., Guo, H. L., Zhao, L. N., & Sun, X. F. (2011). Supplemental selenium alleviates the toxic effects of excessive iodine on thyroid. Biological trace element research, 141(1-3), 110–118. https://doi.org/10.1007/s12011-010-8728-8
- Mizokami, T., Wu Li, A., El-Kaissi, S., & Wall, J. R. (2004). Stress and thyroid autoimmunity. Thyroid : official journal of the American Thyroid Association, 14(12), 1047–1055. https://doi.org/10.1089/thy.2004.14.1047
- Lerner, A., Jeremias, P., & Matthias, T. (2017). Gut-thyroid axis and celiac disease. Endocrine connections, 6(4), R52–R58. https://doi.org/10.1530/EC-17-0021
- Balhara, Y. P., & Deb, K. S. (2013). Impact of alcohol use on thyroid function. Indian journal of endocrinology and metabolism, 17(4), 580–587. https://doi.org/10.4103/2230-8210.113724
- Sachmechi, I., Khalid, A., Awan, S. I., Malik, Z. R., & Sharifzadeh, M. (2018). Autoimmune Thyroiditis with Hypothyroidism Induced by Sugar Substitutes. Cureus, 10(9), e3268. https://doi.org/10.7759/cureus.3268